AIRWAY PART III – ADVANCED AIRWAY ADJUNCTS
ISSN-1059-6518
Part III of the Airway Series – Advanced Airway Adjuncts
By Frank Hubbell, DO
Illustrations by T.B.R. Walsh
In this section we will discuss the use of the endotracheal tube and the remaining airway adjuncts.
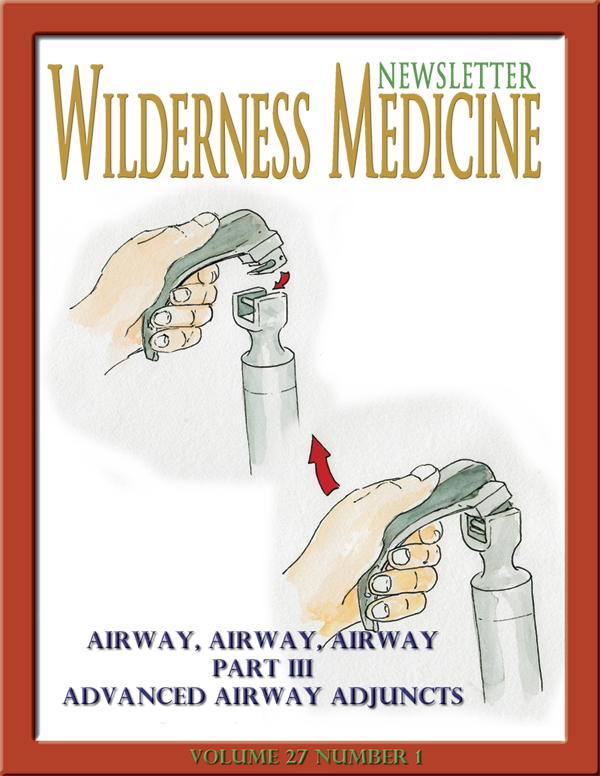
Endotracheal Intubation (ETT)
Gum Elastic Bougie/Flex-Guide Tube Introducers
Digital Intubation
Nasopharyngeal Intubation
Suction
Pulse Oximetry
Capnography and End-Tidal CO₂ detectors (EtCO₂)
CPAP
Stoma and Tracheostomy Care
TOTAL AIRWAY CONTROL – Endotracheal Intubation:
Last, but not least, of the airway adjuncts is endotracheal tube (ETT) intubation.
This is the most advanced airway, and it provides the greatest protection for the airway. This airway technique requires the most knowledge of airway anatomy and many hours of practice to develop the skills of using it. This is also a classic example of a, “use it or lose it” skill, requiring frequent live ETT intubations or practice on airway manikins.
ENDOTRACHEAL TUBE INTUBATION: (ETT)
Indications:
Respiratory or cardiac arrest
Unconscious without a gag reflex
Rapidly deteriorating respirations or impending respiratory failure
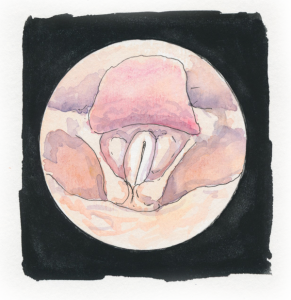
Glottis seen through laryngoscopy
Significant risk of aspiration from vomiting and obtundation
Potential airway obstruction from trauma, burns, or anaphylaxis
Contraindications:
Epiglottitis (patient is sitting up, in the sniff position, and drooling).
Head, neck, or facial trauma that prevents visualization of the airway anatomy.
Advantages of Endotracheal Intubation:
Complete control of the airway.
Isolates the airway.
Minimizes the risk of aspiration of gastric contents.
Eliminates the need to maintain a mask seal.
Allows direct suctioning of the trachea and respiratory passages.
It permits administration of some medications via the endotracheal tube –
naloxone, atropine, vasopressin (adults), epinephrine, and lidocaine.
Disadvantages of endotracheal intubation:
The techniques require considerable training and ongoing practice.
Intubation requires specific equipment.
Typically it is necessary to directly visualize the vocal cords.
Intubation bypasses the upper airway, and its functions of cleaning, warming, and
humidifying the air en route to the alveoli.
Complications of endotracheal intubation:
Risk of equipment malfunction
Soft tissue damage
Broken teeth
Esophageal intubation
Tension pneumothorax
Endobronchial intubation (tube advanced too far into the right or left mainstem bronchus)
Breath sounds present on one side of the chest, diminished on the other side.
Resistance to ventilations with a bag-valve-mask (BVM).
Pallor, cyanosis, evidence of hypoxia.

