Medications That an EMT Can Administer or Help Administer
ISSN-1059-6518
The Backpack or Traveling Pharmacy
By Frank Hubbell, DO
A group of long time friends, three couples and various children, were always coming up with new adventures to share. One of the couples loves to sail and suggested that they should all get together and rent a sailboat for a couple of days and go for an ocean voyage. Over the next several months that idea for a great vacation grew, as did their enthusiasm. They eventually were able to rent a sailboat along with its captain in the US Virgin Islands for their Great Adventure. The ship could accommodate all ten of them for a grand week of cruising on the great blue Caribbean sea.
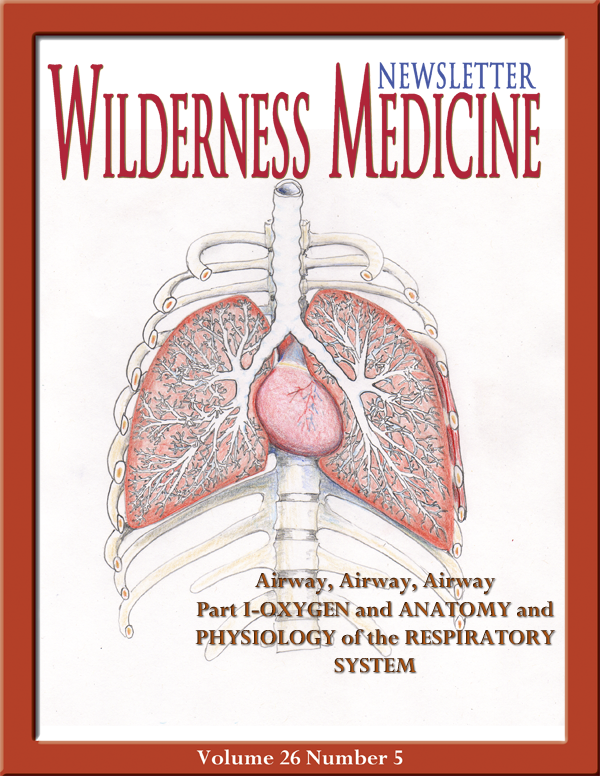
Off they went to the Caribbean and for the first three days all went well. In the evening of the forth day, several of the younger kids began to feel sick with scratchy, burning throats, itchy eyes, runny noses, and upset stomachs. Because they were all in such close quarters the adults decided that the kids were either coming down with colds or allergies. Over the next several hours their conditions worsened and two of the kids began to complain of a sensation of shortness of breath accompanied by wheezing. At the same time several of the adults confessed that they were also beginning to fell sick, with similar symptoms. One of the adults complained of a burning, peppery taste in her mouth. Obviously, they were all getting progressively alarmed.
After sailing all day, the group was now anchored in a nice little hurricane hole on a remote uninhabited island. They would have to wait until morning to head for the nearest port, about four hours away once under sail.
A call was placed to the US Coast Guard who after listening to all the symptoms, thought it might be scombroid poisoning from eating fish that was not properly stored and refrigerated. They explained that it was a form of histamine overdose from eating the fish, in this case mahi mahi, and they needed to treat everyone onboard with antihistamines plus anyone who was wheezing would also need use a rescue inhaler, a bronchodilator such as albuterol.
There were no pharmacists, nurses, EMTs, or docs on board. The group needed to figure this out themselves. They decided to gather all the medications that each of them had brought and see what they had that might be of help. What would have helped the most was good old fashioned KNOW HOW. By the way, no internet service was available, just advice from the Coast Guard via their marine radio that the Captain was required to have on board the boat. (And no, the boat was not the USS Minnow on a 3-hour tour.)
This article highlights standard information that is taught to EMTs. The medications mentioned are ones they can and will commonly use in providing emergency medical care. Some of these medications are over-the-counter meds while others are prescription meds. The following section covers the basic pharmacological aspects of EMT training.