What is a SOAP Note?

November/December 2011 ISSN-1059-6518 Volume 24 Number 6
What is a SOAP Note?
By Frank Hubbell, DO
Illustrations by T.B.R. Walsh
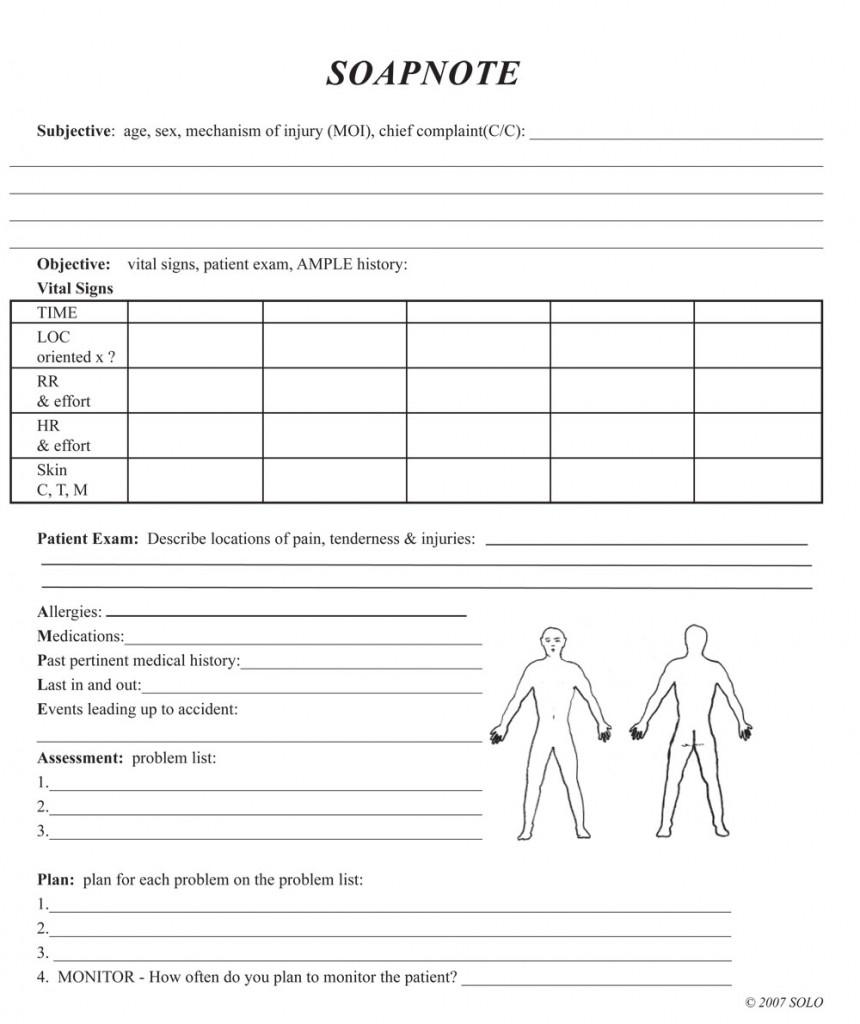
When providing patient care you have a lot of information to gather about the patient including; their past medical history, the chief complaint, vital signs, injuries, and treatment plan. As this information is gathered, it has to be organized, recorded, and able to be mobile. (Mobile in that it has to be able to travel with the patient as they move from the location of the crisis, into an ambulance, and delivered to a definitive care setting.)
The SOAP Note was developed years ago, and today it is a standardized method for organizing all of the patient’s medical information. For many years the SOAP Note has been recognized as the standard for collecting and recording patient data. As a result, it is universally recognized by pre-hospital as well as hospital-based personnel.
Use of the SOAP Note also makes it much easier to communicate, as everyone is using the same template, knows how the information will flow, and where data will be located within the structure of the document.
The SOAP note is organized into Subjective, Objective, Assessment, and Plan.
