Part III of the Airway Series – Advanced Airway Adjuncts
By Frank Hubbell, DO
Illustrations by T.B.R. Walsh
In this section we will discuss the use of the endotracheal tube and the remaining airway adjuncts.
Endotracheal Intubation (ETT)
Gum Elastic Bougie/Flex-Guide Tube Introducers
Digital Intubation
Nasopharyngeal Intubation
Suction
Pulse Oximetry
Capnography and End-Tidal CO₂ detectors (EtCO₂)
CPAP
Stoma and Tracheostomy Care
TOTAL AIRWAY CONTROL – Endotracheal Intubation:
Last, but not least, of the airway adjuncts is endotracheal tube (ETT) intubation.
This is the most advanced airway, and it provides the greatest protection for the airway. This airway technique requires the most knowledge of airway anatomy and many hours of practice to develop the skills of using it. This is also a classic example of a, “use it or lose it” skill, requiring frequent live ETT intubations or practice on airway manikins.
ENDOTRACHEAL TUBE INTUBATION: (ETT)
Indications:
Respiratory or cardiac arrest
Unconscious without a gag reflex
Rapidly deteriorating respirations or impending respiratory failure
Glottis seen through laryngoscopy
Significant risk of aspiration from vomiting and obtundation
Potential airway obstruction from trauma, burns, or anaphylaxis
Contraindications:
Epiglottitis (patient is sitting up, in the sniff position, and drooling).
Head, neck, or facial trauma that prevents visualization of the airway anatomy.
Advantages of Endotracheal Intubation:
Complete control of the airway.
Isolates the airway.
Minimizes the risk of aspiration of gastric contents.
Eliminates the need to maintain a mask seal.
Allows direct suctioning of the trachea and respiratory passages.
It permits administration of some medications via the endotracheal tube –
naloxone, atropine, vasopressin (adults), epinephrine, and lidocaine.
Disadvantages of endotracheal intubation:
The techniques require considerable training and ongoing practice.
Intubation requires specific equipment.
Typically it is necessary to directly visualize the vocal cords.
Intubation bypasses the upper airway, and its functions of cleaning, warming, and
humidifying the air en route to the alveoli.
Complications of endotracheal intubation:
Risk of equipment malfunction
Soft tissue damage
Broken teeth
Esophageal intubation
Tension pneumothorax
Endobronchial intubation (tube advanced too far into the right or left mainstem bronchus)
Breath sounds present on one side of the chest, diminished on the other side.
Resistance to ventilations with a bag-valve-mask (BVM).
Krokodil sounds wild, but in this case it is not necessarily a wilderness or backcountry type article. Unfortunately, some people do like to wander off into the wilderness seeking a high that is more than what Mother Nature can supply. It is not unreasonable to have to deal with drugs and/or a drug overdose situation as part of a mountain or wilderness rescue.
It has been recently reported in the press that the use of heroin is on the rise, and one of its competitors, Krokodil, is also. Krokodil is a very dirty street drug, and it is now here in our towns.
There are those that say all the press this street drug is getting is just a lot of hype. Hype or not, the fact is that according to DAWN, the Drug Abuse Warning Network, 35% of all ER visits relate to or are a result of the use of opiates. We do not want to be victims of “hype,” but we have to be aware that it is out there, and we have to know how to recognize and deal with it.
KROKODIL – CROCODILE – DESOMORPHINE
“The Zombie Drug” the “Flesh Eating Drug,” both well earned nicknames.
The purpose of airway adjuncts is to maintain a patent, open airway. This is accomplished primarily by preventing the tongue or other soft tissues from occluding the entrance to the airway at the larynx.
These airway adjuncts are divided into three categories.
1.There are primary airways for immediate support of the airway
2.Intermediate airways designed for longer-term use.
3.Total airway control airways, which require endotracheal intubation that not only maintain an open, patent airway, but also help to prevent aspiration of fluids into the lungs.
REMEMBER: Primary and intermediate airway adjuncts do not necessarily prevent the aspiration of saliva, blood, vomitus, or other fluids from getting into the trachea and lungs.
IMMEDIATE TECHNIQUES for ESTABLISHING andMAINTAINING an OPEN AIRWAY:
PRIMARY AIRWAYS:
The RECOVERY POSITION:
This is the quickest and simplest way to establish and maintain an open airway in an unconscious patient. You simply have to know how to properly safely logroll someone onto his or her side.
1.When the need for emergency airway management arises, it is usually a scene that is already difficult, desperate, rapidly deteriorating. A scene that most likely requires critical care skills. One of those rare times where speed is of the essence.
2.Your patient may be unruly, uncooperative, or even intoxicated.
3.Your patient will most likely already be hypoxic with poor oxygenation and decreasing respiratory and ventilatory efforts. As a result they will not tolerate even short periods of apnea or hypoxia.
4.Your patient may have recently eaten or drank, and these stomach contents dramatically increase the risk of vomiting and with the risk of aspiration.
5.Their airway may already be compromised by blood, vomitus, secretions, or distorted anatomy from trauma.
6.Your patient may be a cardiac arrest or a near-arrest situation.
OXYGEN: Let’s begin this discussion with oxygen.
When we talk about the importance of maintaining an open airway, what we are really talking about is the importance of a constant, uninterrupted flow of oxygen to every cell in the body. The cells with the greatest demand, and therefore the most sensitive tissues to oxygen supply, are the nerve cells that make up the brain. These neurological tissues can only survive intact for 4 – 6 minutes without oxygen; after 10 minutes without
O2 , irreversible brain damage occurs and most likely death.
The human brain makes up 2% of our total body weight, but it is hypermetabolic:
https://www.wildernessmedicinenewsletter.com/wp-content/uploads/2014/10/wmnlogo20151.png00WMN Editorshttps://www.wildernessmedicinenewsletter.com/wp-content/uploads/2014/10/wmnlogo20151.pngWMN Editors2013-12-04 20:52:282014-01-14 20:11:08AIRWAY PART I: ANATOMY and PHYSIOLOGY of the RESPIRATORY SYSTEM
AIRWAY PART III – ADVANCED AIRWAY ADJUNCTS
/in Airway, Face, Medical Response/by WMN EditorsISSN-1059-6518
Part III of the Airway Series – Advanced Airway Adjuncts
By Frank Hubbell, DO
Illustrations by T.B.R. Walsh
In this section we will discuss the use of the endotracheal tube and the remaining airway adjuncts.
Endotracheal Intubation (ETT)
Gum Elastic Bougie/Flex-Guide Tube Introducers
Digital Intubation
Nasopharyngeal Intubation
Suction
Pulse Oximetry
Capnography and End-Tidal CO₂ detectors (EtCO₂)
CPAP
Stoma and Tracheostomy Care
TOTAL AIRWAY CONTROL – Endotracheal Intubation:
Last, but not least, of the airway adjuncts is endotracheal tube (ETT) intubation.
This is the most advanced airway, and it provides the greatest protection for the airway. This airway technique requires the most knowledge of airway anatomy and many hours of practice to develop the skills of using it. This is also a classic example of a, “use it or lose it” skill, requiring frequent live ETT intubations or practice on airway manikins.
ENDOTRACHEAL TUBE INTUBATION: (ETT)
Indications:
Respiratory or cardiac arrest
Unconscious without a gag reflex
Rapidly deteriorating respirations or impending respiratory failure
Glottis seen through laryngoscopy
Significant risk of aspiration from vomiting and obtundation
Potential airway obstruction from trauma, burns, or anaphylaxis
Contraindications:
Epiglottitis (patient is sitting up, in the sniff position, and drooling).
Head, neck, or facial trauma that prevents visualization of the airway anatomy.
Advantages of Endotracheal Intubation:
Complete control of the airway.
Isolates the airway.
Minimizes the risk of aspiration of gastric contents.
Eliminates the need to maintain a mask seal.
Allows direct suctioning of the trachea and respiratory passages.
It permits administration of some medications via the endotracheal tube –
naloxone, atropine, vasopressin (adults), epinephrine, and lidocaine.
Disadvantages of endotracheal intubation:
The techniques require considerable training and ongoing practice.
Intubation requires specific equipment.
Typically it is necessary to directly visualize the vocal cords.
Intubation bypasses the upper airway, and its functions of cleaning, warming, and
humidifying the air en route to the alveoli.
Complications of endotracheal intubation:
Risk of equipment malfunction
Soft tissue damage
Broken teeth
Esophageal intubation
Tension pneumothorax
Endobronchial intubation (tube advanced too far into the right or left mainstem bronchus)
Breath sounds present on one side of the chest, diminished on the other side.
Resistance to ventilations with a bag-valve-mask (BVM).
Pallor, cyanosis, evidence of hypoxia.
Read more
KROKODIL – Desomorphine
/in Poisons, prevention/by WMN EditorsISSN-1059-6518 Volume 26 Number 6
IS IT ALL HYPE? or IS THE CONCERN REAL?
By Frank Hubbell D.O.
Krokodil sounds wild, but in this case it is not necessarily a wilderness or backcountry type article. Unfortunately, some people do like to wander off into the wilderness seeking a high that is more than what Mother Nature can supply. It is not unreasonable to have to deal with drugs and/or a drug overdose situation as part of a mountain or wilderness rescue.
It has been recently reported in the press that the use of heroin is on the rise, and one of its competitors, Krokodil, is also. Krokodil is a very dirty street drug, and it is now here in our towns.
There are those that say all the press this street drug is getting is just a lot of hype. Hype or not, the fact is that according to DAWN, the Drug Abuse Warning Network, 35% of all ER visits relate to or are a result of the use of opiates. We do not want to be victims of “hype,” but we have to be aware that it is out there, and we have to know how to recognize and deal with it.
KROKODIL – CROCODILE – DESOMORPHINE
“The Zombie Drug” the “Flesh Eating Drug,” both well earned nicknames.
Read more
AIRWAY PART II: EMERGENCY AIRWAY MANAGEMENT
/in Airway, Face, Medical Response, Respiratory System, Trauma/by WMN EditorsISSN-1059-6518
AIRWAY-PART II – EMERGENCY AIRWAY MANAGEMENT
By Frank Hubbell, DO
Illustrations by T.B.R. Walsh
The PURPOSE of Airway Adjuncts:
The purpose of airway adjuncts is to maintain a patent, open airway. This is accomplished primarily by preventing the tongue or other soft tissues from occluding the entrance to the airway at the larynx.
These airway adjuncts are divided into three categories.
1. There are primary airways for immediate support of the airway
2. Intermediate airways designed for longer-term use.
3. Total airway control airways, which require endotracheal intubation that not only maintain an open, patent airway, but also help to prevent aspiration of fluids into the lungs.
REMEMBER: Primary and intermediate airway adjuncts do not necessarily prevent the aspiration of saliva, blood, vomitus, or other fluids from getting into the trachea and lungs.
IMMEDIATE TECHNIQUES for ESTABLISHING and MAINTAINING an OPEN AIRWAY:
PRIMARY AIRWAYS:
The RECOVERY POSITION: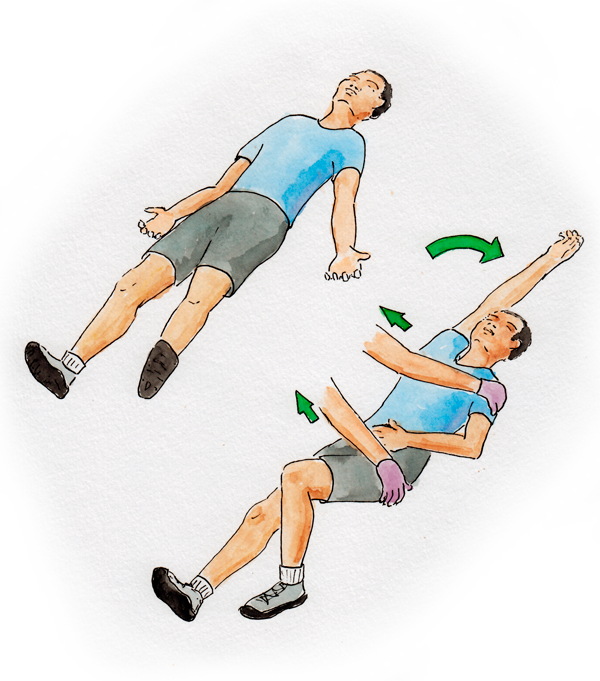
This is the quickest and simplest way to establish and maintain an open airway in an unconscious patient. You simply have to know how to properly safely logroll someone onto his or her side.
Read more
AIRWAY PART I: ANATOMY and PHYSIOLOGY of the RESPIRATORY SYSTEM
/in Airway, Allergies, Asthma, Oxygen, Respiratory System, Shortness of breath/by WMN EditorsISSN-1059-6518
The Challenges of Emergency Airway Management:
By Frank Hubbell, DO
Illustrations by T.B.R. Walsh
First, let’s define the problem:
1. When the need for emergency airway management arises, it is usually a scene that is already difficult, desperate, rapidly deteriorating. A scene that most likely requires critical care skills. One of those rare times where speed is of the essence.
2. Your patient may be unruly, uncooperative, or even intoxicated.
3. Your patient will most likely already be hypoxic with poor oxygenation and decreasing respiratory and ventilatory efforts. As a result they will not tolerate even short periods of apnea or hypoxia.
4. Your patient may have recently eaten or drank, and these stomach contents dramatically increase the risk of vomiting and with the risk of aspiration.
5. Their airway may already be compromised by blood, vomitus, secretions, or distorted anatomy from trauma.
6. Your patient may be a cardiac arrest or a near-arrest situation.
OXYGEN: Let’s begin this discussion with oxygen.
When we talk about the importance of maintaining an open airway, what we are really talking about is the importance of a constant, uninterrupted flow of oxygen to every cell in the body. The cells with the greatest demand, and therefore the most sensitive tissues to oxygen supply, are the nerve cells that make up the brain. These neurological tissues can only survive intact for 4 – 6 minutes without oxygen; after 10 minutes without
O2 , irreversible brain damage occurs and most likely death.
The human brain makes up 2% of our total body weight, but it is hypermetabolic:
– it requires 15% of our cardiac output,
– 20% of total body oxygen consumption, and
– 25% of the total body utilization of glucose.
Read more